Role of Radiotherapy and Radiosurgery for Brain Metastases
Episodes in this series
Priscilla Brastianos, MD: Let’s talk about treatment options. I want to highlight how important multidisciplinary care is for the management of these patients.
Raymond Sawaya, MD: The overarching points related to treating brain metastases are effectiveness and quality of life. We could do things like give very high dose of radiation that may be effective but could harm the patient. First and foremost in our decision-making is how can we maximize the effectiveness and minimize the side effects. To give you a specific example, when you get a large brain metastasis—by large, I mean over an inch, over 3 cm—although radiation could help, it may not be as effective as having the tumor removed and then radiation provided. This way, you minimize the side effects and you increase the effectiveness of the therapy.
Priscilla Brastianos, MD: Talk to us about the radiation, the radiosurgery options for patients, and tell us a little about the modalities.
Raymond Sawaya, MD: From a focal therapy, this is a general term used when we apply very localized therapy—in particular, surgery or stereotactic radiosurgery [SRS]. The benefit of SRS is that it is noninvasive. That’s a great advantage and benefit for patients because we are not admitting them to the hospital. We do the procedure as an outpatient setup, and the patient is home the same day. The question is when is radiosurgery preferable to surgery, and when is surgery preferable to radiosurgery? That goes back to the concept of effectiveness and side effects. The larger the tumor, the less effective is SRS. You have to balance the size or the volume of the metastasis and the number of metastases because some patients will have more than one metastasis.
The larger the tumor, the better it is to apply surgery first and then radiation, most likely radiosurgery. If the tumors are small—and by small, I mean less than 1 inch, less than 2½ cm in diameter—then radiosurgery becomes an excellent option with high rate of local control, meaning the tumor would remain without growth or even shrink or sometimes disappear. That’s the goal of the treatment: to be effective in stopping the tumor from growing and not causing damage to the surrounding brain.
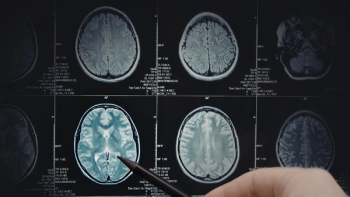
Vinai Gondi, MD: Radiotherapy is remarkably effective for lesions in the brain. One of the things that has been fun to be a part of in the last 10 years is we’ve made a number of innovations in the delivery of radiotherapy to maintain that effectiveness but also to do it more safely for our patients. In general, we break it into two broad categories when we’re deliberating therapies: the delivery of focal radiotherapy to gross macrometastatic disease, meaning lesions that we can visualize on an MRI. Keep in mind, it takes almost a billion cells for a tumor to show up on an MRI. For it to actually be there means there’s a lot of tumor cancer cells in that focus.
Then there’s the micro metastatic disease, meaning it’s not visible on the MRI. The fact is that—to Ivy Elkins’ point, or maybe her radiation oncologist’s point—the brain is an organ, so it’s possible for cells to spread elsewhere in the brain. Radiosurgery, the delivery of a high-dose radiation to a focal lesion, treats gross macrometastatic disease. It treats lesions that we can see on an MRI. It doesn’t treat micrometastatic disease, and as a result, it becomes important to follow that brain with MRI surveillance, typically every couple of months after treatment.
One of the great innovations we’ve had in the last five to 10 years is our technology for radiosurgery—a couple of people have mentioned gamma knife radiosurgery. There are a number of modalities for radiosurgery that are widely available and are allowing us to treat more and more lesions safely in a single treatment, which becomes very convenient and also easier for patients undergoing that procedure.
The second option that we think about is something that Ivy mentioned, which is whole-brain radiotherapy, where we’re treating what we see and what we cannot see. We’ve come a long way with whole-brain radiotherapy in the last five years, developing techniques that are sparing the memory zones in the brain, called the hippocampi, and providing certain pharmacological neuroprotectants in the use of a drug—called memantine, or Namenda—that allows us to treat macrometastatic and micrometastatic diseases effectively and safely without some of the cognitive issues that we’ve seen with conventional whole-brain radiotherapy.
Both of those strategies, from a radiotherapy perspective, are available. They’re on the table every time a patient comes in with brain metastases. It’s complementing it in a multidisciplinary manner with all the other therapies that are available, trying to discuss the pluses and minuses and framing it within the context of the goals of care for that particular patient.
Transcript Edited for Clarity