Factors Considered When Selecting Treatment for Brain Metastases
Episodes in this series
Priscilla Brastianos, MD: What factors do you consider when weighing efficacy vs physical and cognitive effects of treatments?
Raymond Sawaya, MD: The whole issue of cognitive impairment is a critical one, and it has become an issue when patients receive whole-brain radiation therapy, something our radiation oncologist will expand on. But because the whole-brain radiation concept has been associated with diminished cognition, diminished memory and executive functioning, most specialists try to avoid whole-brain radiation. Therefore, we go back to the focal therapy, such as surgery plus radiation or radiation alone in a focal way, like stereotactic radiosurgery. When you do that, then it’s very unlikely that the patient will suffer from cognitive deficits because of the treatment.
Priscilla Brastianos, MD: This is now a question for Vinai. You alluded to it a little with the memantine. But tell us a little more about how you weigh patient-reported outcomes with potential treatments. Why don’t you tell us about that?
Vinai Gondi, MD: It’s an area of my research, as you guys know, and something we really try to focus on is how we can optimize that with the radiotherapy approach. There’s no blood-brain barrier for radiotherapy, so that’s helpful. We can treat the lesions in the brain with over 90% control. But there is a recognition of whether radiotherapy should be utilized in a situation. If you have a patient who is going to be on a systemic therapy and has the capacity to offer some activity in the brain, similar to what happened with Ivy Elkins’ situation, then probably the best thing—from a patient-reported-outcomes cognitive perspective—if they’re having no symptoms and they’re small, is to do nothing. From a radiotherapy perspective, it’s better to just follow and see how things go, recognizing that you can keep that tool in your back pocket for some time down the road.
However, there are scenarios, and unfortunately, the majority of patients with brain metastases just don’t have systemic therapy options that do have activity or compelling activity in the brain. If they happen to have lesions in parts of the brain where you get a little question, you wonder: If there’s any more growth, there could be some symptoms that develop. In those scenarios, we weigh the two radiotherapy approaches that work effectively—radiosurgery, but also the whole-brain radiotherapy. We ran a number of clinical trials. We talked about this drug memantine. Research that was published a few years ago showed that we can effectively prevent cognitive toxicity from whole-brain radiotherapy. But even more recently, when we used hippocampal avoidance using IMRT [intensity-modulated radiation therapy], we showed that we can offer even more cognitive protection. Of those results, most important was that we were able to show that patient-reported outcomes were better when they were treated with hippocampal avoidance. It speaks to the ability to control lesions in the brain and the associated symptoms as well as preventing some of those cognitive outcomes.
In my clinic, I’m fortunate to have all these options available to patients, and I go through each one individually. It really depends on the type of cancer. If it’s Ivy’s situation, where she has a systemic therapy that’s very effective, I say, “Hey, looks great. I’ll see you in a couple of months. I think we’ll just watch it.” If it’s Katie Doble’s unfortunate situation, where she had something in a very sensitive area, in the pons, and causing symptoms, we need to act quickly so we can reverse these symptoms. Because there’s only one lesion, we focally treat it and watch carefully.
There are certain scenarios where patients come in with what I call brain-dominant disease. Everything is controlled in the body systemically, but they keep popping up with new lesions in the brain, and we’re chasing our tails a little. To some extent, it speaks to the importance of intracranial control. In those situations, we then think about optimizing that, maybe using hippocampal avoidant whole-brain radiation in those scenarios.
Everybody is different, and every patient is different. One of the unique things about brain metastases, unlike perhaps primary brain tumors, is there are so many histologies that can feed into this machination of brain metastases development. It becomes interesting, it becomes fascinating, but it becomes personalized. We take each patient individually and weigh all those factors.
Raymond Sawaya, MD: The whole concept of “the expert decides, and that’s the end of the story” is old news. We are treating a patient, we are treating a family, and those treatments have to be done in concert with their understanding, with their preference to the extent that they’re able to make the decision. Sometimes they tell us, “Well, you’re the expert, you tell us what to do.” But in reality, most patients and caregivers are quite sophisticated and have done a lot of reading, on Google or otherwise, and they come prepared with excellent and intelligent questions. Our role is to provide the information as we know it. Sometimes we don’t have all the answers, and that takes us into the concept of clinical trial, which I know is very much on your mind and on patients’ minds. We don’t always have the answer, but we share what we know with the patient and come to a decision collectively.
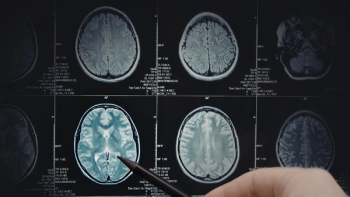
I want to bring up one concept that is beginning to be applied more widely in the United States, and that is the concept of the brain metastasis clinic. Dr Brastianos, our leader today, is very familiar with this concept. It’s worthwhile to share the idea with patients and caregivers. It’s a patient-focused clinic where the patient meets all the specialists who will potentially be involved in their care and their treatment. That includes a medical oncologist, the neuro-oncologist, the neurosurgeon, the radiation oncologist and the neuro-radiologist, because the brain metastasis are usually diagnosed with imaging, with an MRI scan. We need the input of the neuro-radiologist as well to define what is a tumor, what is not a tumor, what may be a scar and what may be swelling. The whole team gets together in one location, where the patient is, and that is the whole idea behind a brain metastasis clinic.
Transcript Edited for Clarity