- Rare Cancers Special Issue
- Volume 1
- Issue 1
Power in the Words: Discussing Palliative Cancer Care
The approach used in discussing palliative care can play a role in whether a patient seeks help.
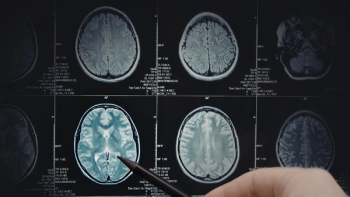
EARLY ON IN HIS career, Andrew Chi, M.D., Ph.D., chief of neurooncology and co-director of the Brain Tumor Center at NYU Langone Health in New York City, learned to be careful in how to introduce his new patients with glioblastoma multiforme (GBM) to palliative care; that is, care that does not seek to cure but to improve pain management and quality of life.
“(The) current consensus is to, ‘Start talking about palliative care early. Be realistic.’ But if you don’t approach those topics carefully with new patients, they may not come back,” Chi explains. “If you’re a young man in your 40s with kids, and you’ve just been diagnosed, most likely you want to talk about fighting, not looking to ease suffering.”
After several patients failed to return for a second visit, Chi changed the way he talked about this issue. “During my initial visits, I often call it ‘supportive oncology,’ instead of palliative care,” he says. “I advise our patients with GBM to see our palliative care practitioners early to talk about social support, depression, pain management, help at home.”
Chi emphasizes that the provider’s role is palliative care. He deemphasizes the association with hospice care, instead focusing on palliation, or alleviation of suffering. Unfortunately, the term palliative care, which nearly all doctors say, has been linked in the public’s mind to hospice and end of life. This leads many patients to fear the concept.
A December 2017 study in Current Oncology found that when patients learned that palliative measures can complement curative treatments, most of them expressed interest in these services.
GBM poses many challenges for patients: Abilities often decline quickly after diagnosis, and treatments can be aggressive.
Neither patients nor their loved ones and caregivers feel they have time to consider social support, mental health and so on when they are dealing with an avalanche of medical information and fighting for life. But doing so can reduce stress and increase quality of life, experts say. Even patients who do well from a standpoint of cancer may continue to live with physical and emotional distress.
“We consider palliative care one of the essential pillars of caring for patients with glioblastoma,” says Vinai Gondi, M.D., director of research and education at Northwestern Medicine Chicago Proton Center in Warrenville, Illinois. “There are a wide range of initiatives seeking to give these patients access to supportive care, how best to help support needs at home.”
Many patients with GBM are too ill to attend support groups and meet with counselors outside the home, explains Richard Dickens, MS, LSW-R, director of client advocacy for CancerCare, a nonprofit organization that provides counseling, education and other support to patients with cancer.
Dickens suggests that patients with GBM join a telephone or online support group to connect with others in a similar situation. CancerCare offers these groups for both patients and caregivers. Online services to coordinate a group of caregivers also are available from other groups, such as Lotsa Helping Hands.
“Patients with GBM have big issues,” explains Sean Grimm, M.D., director of neuro-oncology at Northwestern Medicine Cancer Center, also in Warrenville. “They go from working to not working, they suffer from depression, they need help at home. They need help getting disability. They have neurologic symptoms that require rehab and physical therapy. They need help with nutrition. All (of) these things are important. Palliative care includes all (of) these things.”
Articles in this issue
over 7 years ago
Success in Cancer Care Doesn't Happen Overnightover 7 years ago
Driving Research in Rare Cancersover 7 years ago
Progress in Sarcoma Treatment, But Still a Long Journey Aheadover 7 years ago
Waldenstrom Macroglobulinemia: The Discovery and What Lies Aheadover 7 years ago
Advances and Combinations Raise Sights on Uveal Melanomaover 7 years ago
Turning the Tide in Glioblastoma