Pediatric Neuroblastoma Survivors Face Task Efficiency, Emotional Regulation Impairments
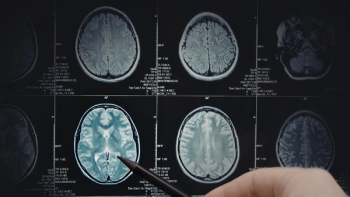
Long-term survivors of pediatric neuroblastoma may be at an increased risk for neurocognitive impairment – in particular, due to age at diagnosis and the type of treatment received.
Long-term survivors of pediatric
“I think what patients should take away from this is that while we may have cured (patients) of their disease, there are long-term consequences to the therapies that we provide,” Caroline Hesko, a pediatric hematology/oncology fellow at The University of Chicago Comer Children's Hospital, said in an interview with CURE. “But with that, even with these patients who have impairments, there are interventions that can be done to help them.”
In their study, Hesko and colleagues collected data from 31 institutions across the United States that included 837 neuroblastoma survivors and 728 of their siblings from 1970 to 1999. Individuals self-reported neurocognitive problems using a
“…The gold standard for (neurocognitive outcomes) is neuropsychological testing, which, for most people, is very difficult to get,” she said. “Even at our center that sees a lot of patients, the wait time to get that testing can be up to nine months. The testing takes a lot of manpower. Not everyone will have access to such testing.”
Overall, the majority of survivors (57%) and their siblings (56%) were female. At the time of study, survivors were a median age of 25 and siblings were 32 years. Median age at diagnosis was 1.
Overall rates for emotional regulation, organization, task efficiency and memory were 19.7%, 25.3%, 21.9% and 19.4%, respectively.
Survivors showed a 50% higher risk for impaired task efficiency and emotional regulation compared with siblings.
Survivors who were less than 1 year at diagnosis, received treatment with platinum-based chemotherapy and experienced hearing loss as well as cardiovascular and neurologic conditions were associated with a higher risk for impaired task efficiency.
Meanwhile, female sex and cardiovascular and respiratory conditions were associated with a higher risk for impaired emotional regulation.
Of survivors who were diagnosed at more than 1 year of age, those treated from 1970 to 1979 had an 80% increased risk for impaired emotional regulation compared with those treated from 1990 to 1999. In addition, hearing loss and respiratory and cardiovascular conditions were associated with a higher risk for task efficiency.
“When we think of task efficiency, we think of processing speed and how fast someone is able to do a task. Those impairments not only depend on age, but also the types of therapies they got. We found that patients who were exposed to platinum-based chemotherapy agents were at higher risk for impairment,” Hesko said, adding that these findings may inform risk-stratified interventions to improve neurocognitive outcomes.
“For example, if a young student is having issues with organizing or processing speed, it may just be that they need extra time in taking their tests or that they may need a different way of organizing their work to be able to help them to succeed. Similarly, knowing that if you're struggling in these areas, figuring out what type of job may be best for you will help you make an informed decision on how to move forward.”