Understanding Your Risk for Brain Metastases
Episodes in this series

Priscilla Brastianos, MD: Ivy and Katie, do you remember your oncologist discussing the risk of brain metastases when you first received your cancer diagnosis?
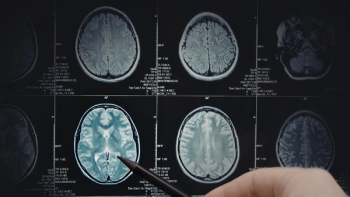
Ivy Elkins: When I was diagnosed, I knew I had stage 4 lung cancer, and initially I had no idea that it could even spread to the brain. I had my PET [positron emission tomography] scan and some other scans done when I was told by my oncology nurse that I should also get a brain MRI [magnetic resonance imaging] to check on things. She told me that there were no indications that it had spread to my brain, but they like to do that for any new stage 4 diagnosis of lung cancer just to make sure. Of course, that made me incredibly nervous because I already found out that I had stage 4 lung cancer, which I didn’t even have any symptoms in my lungs, and now I started worrying about whether I was going to have anything in my brain as well.
When I went for my first appointment with my brand-new thoracic oncologist, who I love and I’ve been with for my entire seven years, that’s when I found out that I had the eight small brain metastases. I was really surprised and shocked, and that changed the discussion from whether I should start on the targeted therapy that they had planned to start me on for my EGFR [epidermal growth factor receptor] mutation, or whether I needed to take care of or treat the brain metastases first. I went that very same day to speak to radiation oncology in the hospital, and I still remember the radiation oncologist who I spoke with — because I was freaking out about having brain metastases — saying to me, “The brain is an organ like other organs and it can be treated like other organs.” That stuck in my mind and I’ve thought of that a number of times since.
At that point, since the targeted therapy, I went on a drug called afatinib; it had been recently FDA approved and no one knew whether it would penetrate the blood-brain barrier and have impact on the metastases in my brain. The radiation oncologist said to me, “We may need to consider brain radiation at some point in the future, possibly whole-brain radiation, because if there’s eight small metastases, there’s a good chance there are others that we haven’t been able to detect.” That obviously wasn’t something that I was happy to hear. I do remember asking about gamma knife surgery, but they thought that there were probably too many brain metastases to make that a possibility.
My oncologist conferred with the radiation oncologist, and together they decided to start me on the targeted therapy and see how I responded. I was very fortunate to have my brain metastases disappear. I almost couldn’t believe it. As a result, I haven’t had any forms of brain radiation.
Priscilla Brastianos, MD: Unfortunately, the experience you described as being shocked with the initial diagnosis of brain metastases is common in the United States. A lot of patients are not aware of brain metastases before they’re diagnosed. Katie, what about your experience? Do you remember your oncologist discussing the risk of brain metastases before you developed them?
Katie Doble: I do not. Do you?
Nick Doble: No.
Katie Doble: I never had a doctor discuss it with me. In fact, the ocular melanoma community is pretty small, and I remember meeting a woman at the Melanoma Research Foundation’s Wings of Hope for Melanoma Gala in Denver, Colorado, in 2017. She said she was also an ocular melanoma patient, and she told me that it had spread to her brain. I remember thinking, “I can’t unhear that. I don’t want to know.” When it happened to me, I had more than one doctor say, “That’s interesting, it doesn’t typically spread to the brain.” I remember thinking, “How can you say that when I know of another patient and I had heard of other patients who had had this experience?” I think in my case, there are so many unknowns in the ocular melanoma world, so it surprised me that these doctors were surprised. But my oncologist, who is treating me here in Denver, Colorado, is a cutaneous melanoma specialist, because there isn’t an ocular melanoma specialist here, and so he was a little more familiar with it. I’m so thankful that he, when I described my symptoms, said we’re going to do this brain MRI. But that was really the first that we had heard of this possibility in the whole experience.
Priscilla Brastianos, MD: One last question before we move on to the next segment. What types of educational materials did you receive related to brain metastases, and what information did you seek out on your own?
Ivy Elkins: Honestly, I didn’t really receive any educational information, I don’t believe. It was all tied up in a very confusing time because I found out I had lung cancer, which I knew nothing about — and then I found out I had brain metastases, which I knew next to nothing about. There was just so much going on. I do remember once I started on my targeted therapy my oncologist said to me that she thought that this would work better. There were two choices of targeted therapy, but the other targeted therapy that was out there and FDA approved for people who had brain metastases.
I do remember going online. I do like to Google and it’s not always good for me. I Google way too much. I read stories about people who did have a targeted therapy medication for lung cancer penetrate the blood-brain barrier and have an impact on their brain, and I read stories where they didn’t. I read some articles about my targeted therapy in scientific journals about that possibility. I pretty much sat back and kept my fingers crossed until my first scan, my first MRI, just to see what would happen, because there really wasn’t anything else I could do at that point. I just remember hoping that this would take care of it and I wouldn’t need to do the radiation.
Priscilla Brastianos, MD: And what about you, Katie?
Katie Doble: I don’t remember getting any specific information about it, and it honestly all happened very quickly. My cutaneous melanoma oncologist called me, and he said, “It’s confirmed and we’re going to have you do gamma knife, we’re scheduling you next week.” I didn’t even meet with the neurologist before I went in for the procedure. My dad, again, flew out so he could be there with us for the procedure. I’m sure that Nick, my dad, my sister and anyone else who knew me was Googling it, but I wasn’t. I just want a high level, what can I expect, but I don’t want to know the nitty-gritty details. But I didn’t get any, not that I recall, do you recall getting?
Nick Doble: No.
Katie Doble: — specific information or pamphlets or anything like that given to us.
Transcript Edited for Clarity