Katie’s Journey With Stage IV Ocular Melanoma That Has Spread to the Brain
Episodes in this series

Priscilla Brastianos, MD: Katie, tell us your story.
Katie Doble: Thank you, first of all, for having us here. Ivy, thank you for sharing your story. It’s always inspiring for me to hear of other stage IV thrivers. Thank you. I am 38 years old, and when I was 31 years old, I was experiencing some issues with my vision. I called my ophthalmologist after a black line sort of danced across my windshield while I was driving one afternoon, and they had me come in the following morning. I went in, and they told me there was a bump on my retina and that it could potentially be a tear, which could be serious, and they wanted me to get into a retina specialist immediately. I went straight to a retina specialist, where I was diagnosed with ocular melanoma. I was by myself that day. I was totally blindsided—I have a lot of eye jokes if you want to hear them—and I didn’t know what to do. I called my sister, who is a nurse and lives in town, and she came to the doctor with me that afternoon, where we went through what this meant and what my options were.
I have always been in the camp of “I don’t want to know.” Some people like to google everything and know everything. I have not once googled ocular melanoma and what that means. But my sister did, and we learned it affects six in 1 million people and that the standard treatment of care is to have plaque therapy to the eyeball. We underwent the radiation to my eyeball shortly after my diagnosis. It was a weeklong radiation, and it left me 100% blind in my left eye. That was it: I became a cancer survivor. They biopsied my cells during the radiation procedure, and they told me that I had a less than 2% chance of metastatic disease. I thought, “I’m good; life goes on. I’m blind in one eye, with no depth perception, but I’m going to be fine.”
A few months later, I met this young man, and we quickly fell in love. A year later, I went in for a routine liver ultrasound, which was what they had suggested as follow-up care. I had had one in April that year that was totally clean. I went in, it was November 2014, and I got a call that afternoon from the oncologist herself telling me that I had 12 suspicious lesions on my liver, that it was likely that I had fallen into that 2% category and that it had metastasized. We had a liver biopsy. My dad flew out the next day and was there for my liver biopsy—my dad is an internist in Omaha, Nebraska—and it was confirmed that I had developed stage IV cancer.
My oncologist told me, “You’ll get started on Yervoy [ipilimumab], the only FDA-approved drug for your disease. We’ll get you started next week.” My dad said, “That’s not good enough. I want to know if clinical trial options are available.” That doctor replied, “That would be really expensive.” We left her office that day, and my dad was on the phone with every single doctor across America who would speak with him about my case. He presented my case to the tumor board of Nebraska, and he got in touch with some doctors at Memorial Sloan Kettering Cancer Center about a clinical trial there. I never talked to that doctor again. If she saw me today, she might think she saw a ghost. But I started in January 2015 at Sloan Kettering for my first clinical trial. Two days after my metastatic diagnosis, by the way, Nick proposed, and so we had that going on as well.
I had my first clinical trial in 2015, and by August of that year I was booted from that trial because of tumor growth, and I had my first liver embolization at that point. Actually, sorry, I had a second clinical trial at the University of Colorado here in Denver and was booted from that trial as well. I’m good at getting in and out of trials. So, that trial I was booted from. I did a liver embolization, which is a targeted therapy to the liver, and I’ve responded well to that. They treated only half my liver because they wanted to have a baseline to see how I would respond.
I went about six months in 2016 getting a break from treatment, which was glorious, and then in June 2016, there was additional growth. I entered my third clinical trial, and I was in that trial for about three months when there was growth again, and the doctor said, “We want you to go back and have the rest of your liver embolized because you’ve responded very well to that therapy.” I went back and I got the other half of my liver, had the embolization done, and then 2017 was great. We finally took our honeymoon—I had no treatment that year; it was a great year. And 2018 was going really well. I was living with stage IV cancer, but you never would have guessed it.
But midyear 2018, I started presenting with stroke-like symptoms. I remember one morning getting out of bed and feeling like a drunken sailor on a ship that was in the middle of a storm. Everything was moving. I was clipping door frames, trying to go up the stairs was a huge effort—I kept tripping. I knew something was wrong with me, but I didn’t know what was going on with me.
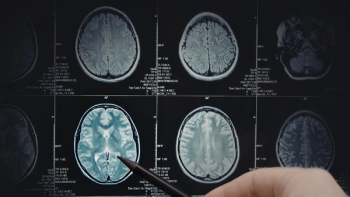
Nick and I carpool to work sometimes, and I was driving us into work and we got rear-ended. I remember thinking, “I can’t even get out of the car right now. I can’t deal with anything.” I thought I was just dehydrated. I had scans the following week, and I mentioned what was going on to my oncologist. He said, “We should get a brain MRI.” Sure enough, something showed up in the left pons—as if I know where that is—and then we found out that it was likely a brain tumor. It’s still unknown; they didn’t biopsy it. I underwent gamma knife the following week, and my brain has been stable since. I had been, as of earlier this year, doing great. I was stable nearly two years in my brain, I had been stable in my liver for about three and a half years.
But on brand with 2020, my scan showed massive growth in my tumors in my liver earlier this year. I ended up enrolling in my fourth clinical trial at the University of Pittsburgh Medical Center and that was TIL [tumor-infiltrating lymphocyte] therapy. I went to Pittsburgh; we went for the month of September and I was in the hospital most of the month. Got my free haircut, got my TIL, and got my IL-2. We just got off the phone with the doctors this morning before this call to get my updated results from my latest scan, and things are going well. The tumors are slightly shrinking, and so we’re pleased with the results. That is, in a nutshell, what we’ve been doing the last seven and a half years.
Priscilla Brastianos, MD: That’s an incredible story. Thank you for sharing that. I’m thrilled that things are going well with this trial.
Transcript Edited for Clarity